- 1 INDICATIONS AND USAGE
- 2 DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 11 DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
1 INDICATIONS AND USAGE
FRUZAQLA is indicated for the treatment of adult patients with metastatic colorectal cancer (mCRC) who have been previously treated with fluoropyrimidine-, oxaliplatin-, and irinotecan-based chemotherapy, an anti-VEGF therapy, and, if RAS wild-type and medically appropriate, an anti-EGFR therapy.
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
The recommended dose of FRUZAQLA is 5 mg orally once daily for the first 21 days of each 28-day cycle until disease progression or unacceptable toxicity. Take FRUZAQLA with or without food [see Clinical Pharmacology (12.3)] at approximately the same time each day.
Swallow the FRUZAQLA capsule whole.
Take a missed dose if less than 12 hours have passed since the missed scheduled dose. Do not take two doses on the same day to make up for a missed dose.
Do not take an additional dose if vomiting occurs after taking FRUZAQLA but continue with the next scheduled dose.
2.2 Dosage Modifications for Adverse Reactions
The recommended dose reductions for adverse reactions are provided in Table 1.
Table 1: Recommended Dose Reductions for FRUZAQLA
| Dose Level | [FRUZAQLA DOSE] |
| First dose reduction | 4 mg orally once daily |
| Second dose reduction | 3 mg orally once daily |
Permanently discontinue FRUZAQLA in patients unable to tolerate 3 mg orally once daily.
The recommended dosage modifications for adverse reactions are provided in Table 2.
Table 2: Recommended Dosage Modifications for FRUZAQLA
| Adverse Reaction | Severity1 | FRUZAQLA Dosage Modification |
| Hypertension [see Warnings and Precautions (5.1)] | Grade 3 |
|
| Grade 4 | Permanently discontinue FRUZAQLA. | |
| Hemorrhagic Events [see Warnings and Precautions (5.2)] | Grade 2 |
|
| Grade 3 or Grade 4 | Permanently discontinue FRUZAQLA. | |
| Hepatotoxicity [see Warnings and Precautions (5.5)] | Alanine aminotransferase (ALT) or aspartate aminotransferase (AST) greater than 3 times upper limit of normal (ULN) with total bilirubin less than or equal to 2 times ULN |
|
| ALT or AST greater than 3 times ULN with concurrent total bilirubin greater than 2 times ULN (in the absence of cholestasis or hemolysis) | Permanently discontinue FRUZAQLA. | |
| AST or ALT greater than 20 times ULN or bilirubin greater than 10 times ULN | Permanently discontinue FRUZAQLA. | |
| Proteinuria [see Warnings and Precautions (5.6)] | 2 grams or greater proteinuria in 24 hours |
|
| Palmar-plantar erythrodysesthesia (PPE) [see Warnings and Precautions (5.7)] | Grade 2 |
|
| Grade 3 |
|
|
| Other Adverse Reactions [see Adverse Reactions (6.1)] | Grade 3 |
|
| Grade 4 | Discontinue FRUZAQLA. Consider resuming FRUZAQLA at the next lower dose level only if the toxicity is non-life threatening and fully resolves or recovers to Grade 1 and the potential benefit outweighs the risks. |
1 Severity as defined by National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE) version 5.0.
3 DOSAGE FORMS AND STRENGTHS
Capsules:
- 1 mg: size 3 hard gelatin capsule with standard yellow opaque cap and white opaque body, imprinted with “HM013” over “1 mg” on the body in black ink.
- 5 mg: size 1 hard gelatin capsule with a red opaque cap and white opaque body, imprinted with “HM013” over “5 mg” on the body in black ink.
4 CONTRAINDICATIONS
None.
5 WARNINGS AND PRECAUTIONS
5.1 Hypertension
FRUZAQLA can cause hypertension. Hypertension occurred in 450 of 911 (49%) patients with mCRC treated with FRUZAQLA, including Grade 3-4 events in 19%, and hypertensive crisis in three patients (0.3%). The median time to first onset of hypertension was 14 days from first dose of FRUZAQLA.
Do not initiate FRUZAQLA unless blood pressure is adequately controlled. Monitor blood pressure weekly the first month, at least monthly thereafter and as clinically indicated. Initiate or adjust anti-hypertensive therapy as appropriate. Withhold, reduce dose, or permanently discontinue FRUZAQLA based on the severity of hypertension [see Dosage and Administration (2.2)]
5.2 Hemorrhagic Events
FRUZAQLA can cause serious hemorrhagic events, which may be fatal. In 911 patients with mCRC treated with FRUZAQLA, 6% of patients experienced a gastrointestinal hemorrhage, including 13 patients (1%) with a Grade ≥3 event and 2 patients with fatal hemorrhages.
Permanently discontinue FRUZAQLA in patients with severe or life-threatening hemorrhage. Monitor the International Normalized Ratio (INR) levels in patients receiving anticoagulants [see Dosage and Administration (2.2)].
5.3 Infections
FRUZAQLA can cause an increased risk of infections, including fatal infections. In 781 patients treated with FRUZAQLA across three randomized, placebo-controlled trials, the overall incidence of infections was higher (18% vs. 12%) including for fatal infections (1% vs. 0.3%) as compared to the placebo arms (n=391).
In 911 patients with mCRC treated with FRUZAQLA, the most common infections were urinary tract infections (6.8%), upper respiratory tract infections (3.2%) and pneumonia (2.5%); fatal infections included pneumonia (0.4%), sepsis (0.2%), bacterial infection (0.1%), lower respiratory tract infection (0.1%), and septic shock (0.1%).
Withhold FRUZAQLA for Grade 3 or 4 infections, or worsening infection of any grade. Resume FRUZAQLA at the same dose when the infection has resolved.
5.4 Gastrointestinal Perforation
FRUZAQLA can cause gastrointestinal perforation. In 911 patients with mCRC treated with FRUZAQLA, 12 patients (1.3%) experienced a Grade ≥3 gastrointestinal perforation, including one fatal event.
Permanently discontinue FRUZAQLA in patients who develop gastrointestinal perforation or fistula.
5.5 Hepatotoxicity
FRUZAQLA can cause liver injury. In 911 patients with mCRC treated with FRUZAQLA, 48% experienced increased ALT or AST, including Grade ≥3 events in 5%, and fatal events in 0.2%. Median time to first onset of elevated liver enzymes was 29 days from first dose of FRUZAQLA.
Monitor liver function tests (ALT, AST, and bilirubin) before initiation and periodically throughout treatment with FRUZAQLA. Temporarily hold and then reduce or permanently discontinue FRUZAQLA depending on the severity and persistence of hepatotoxicity as manifested by elevated liver function tests [see Dosage and Administration (2.2) and Use in Specific Populations (8.6)].
5.6 Proteinuria
FRUZAQLA can cause proteinuria. In 911 patients with mCRC treated with FRUZAQLA, 36% experienced proteinuria and 2.5% of patients experienced Grade ≥3 events. Median time to first onset of proteinuria was 22 days from first dose of FRUZAQLA.
Monitor for proteinuria before initiation and periodically throughout treatment with FRUZAQLA. For proteinuria ≥2 g/24 hours, withhold FRUZAQLA until improvement to ≤Grade 1 proteinuria, resume FRUZAQLA at a reduced dose. Discontinue FRUZAQLA in patients who develop nephrotic syndrome [see Dosage and Administration (2.2)].
5.7 Palmar-Plantar Erythrodysesthesia (PPE)
FRUZAQLA can cause PPE. In 911 patients with mCRC treated with FRUZAQLA, PPE occurred in 35%, including 8% with Grade 3 events. Median time to first onset of PPE was 19 days from first dose of FRUZAQLA.
Based on severity, withhold FRUZAQLA and then resume at the same or reduced dose [see Dosage and Administration (2.2)].
5.8 Posterior Reversible Encephalopathy Syndrome (PRES)
FRUZAQLA can cause PRES, a syndrome of subcortical vasogenic edema diagnosed by characteristic finding on MRI. PRES occurred in one of 911 patients with mCRC treated with FRUZAQLA.
Perform an evaluation for PRES in any patient presenting with seizures, headache, visual disturbances, confusion or altered mental function. Discontinue FRUZAQLA in patients who develop PRES.
5.9 Impaired Wound Healing
Impaired wound healing can occur in patients who receive drugs that inhibit the vascular endothelial growth factor (VEGF) signaling pathway. In 911 patients with mCRC treated with FRUZAQLA, 1 patient experienced a Grade 2 event of wound dehiscence.
Do not administer FRUZAQLA for at least 2 weeks prior to major surgery.
Do not administer FRUZAQLA for at least 2 weeks after major surgery and until adequate wound healing. The safety of resumption of FRUZAQLA after resolution of wound healing complications has not been established.
5.10 Arterial Thromboembolic Events
FRUZAQLA may increase the risk of arterial thromboembolic events. In 911 patients with mCRC treated with FRUZAQLA, 7 patients (0.8%) experienced an arterial thromboembolic event; additionally, FRUZAQLA studies excluded patients with clinically significant cardiovascular disease, uncontrolled hypertension, or with thromboembolic events within the prior 6 months. Initiation of FRUZAQLA in patients with a recent history of thromboembolic events should be carefully considered. In patients who develop arterial thromboembolism discontinue FRUZAQLA.
5.11 Allergic Reactions to FD&C Yellow No. 5 (Tartrazine) and No. 6 (Sunset Yellow FCF)
FRUZAQLA 1 mg capsules contain FD&C Yellow No. 5 (tartrazine), which may cause allergic-type reactions (including bronchial asthma) in certain susceptible persons. Although the overall incidence of FD&C Yellow No. 5 (tartrazine) sensitivity in the general population is low, it is frequently seen in patients who also have aspirin hypersensitivity.
FRUZAQLA 1 mg contains FD&C Yellow No. 6 (sunset yellow FCF), which may cause allergic reactions.
5.12 Embryo-Fetal Toxicity
Based on findings in animal studies and its mechanism of action, FRUZAQLA can cause fetal harm when administered to pregnant women. In an embryo-fetal developmental study in rats, embryotoxic and teratogenic effects were observed at exposures below the clinical exposure [see Use in Specific Populations (8.1)].
Advise pregnant women of the potential risk to a fetus. Advise females of childbearing potential and males with female partners of childbearing potential to use effective contraception during treatment with FRUZAQLA and for 2 weeks after the last dose [see Use in Specific Populations (8.1, 8.3)].
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Hypertension [see Warnings and Precautions (5.1)]
- Hemorrhagic Events [see Warnings and Precautions (5.2)]
- Infections [see Warnings and Precautions (5.3)]
- Gastrointestinal Perforation [see Warnings and Precautions (5.4)]
- Hepatotoxicity [see Warnings and Precautions (5.5)]
- Proteinuria [see Warnings and Precautions (5.6)]
- Palmar-Plantar Erythrodysesthesia (PPE) [see Warnings and Precautions (5.7)]
- Posterior Reversible Encephalopathy Syndrome (PRES) [see Warnings and Precautions (5.8)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The pooled safety population described in the WARNINGS AND PRECAUTIONS and below reflects exposure to FRUZAQLA as a single agent in 911 patients with mCRC who were enrolled in three randomized, placebo-controlled studies (FRESCO-2, FRESCO and 2012-013-00CH1) (N=781); three open-label studies (2009-013-00CH1, 2012-013-00CH3 and 2015-013-00US1) (N=124); and an open-label lead-in cohort of FRESCO-2 (N=6). Among the 911 patients who received FRUZAQLA, 23% were exposed for 6 months or longer and 3.5% were exposed for greater than one year. These patients received at least one dose of FRUZAQLA at the recommended dosage of 5 mg daily for the first 21 days of each 28-day cycle. The median age was 60 years (range: 23 to 82) and 34% were 65 years of age or older. The most common adverse reactions (incidence ≥20%) that occurred in pooled monotherapy studies were hypertension, PPE, proteinuria, dysphonia, abdominal pain, diarrhea, and asthenia.
Metastatic Colorectal Cancer
FRESCO-2 Study
The safety of FRUZAQLA was evaluated in FRESCO-2, a randomized, double-blind, placebocontrolled study [see Clinical Studies (14.1)]. Patients received either FRUZAQLA 5 mg daily for the
first 21 days of each 28-day cycle plus best supportive care (BSC) (n=456) or matching placebo plus
BSC (n=230).
The median duration of therapy with FRUZAQLA was 3 months (range: 0.3 to 19.1 months).
Serious adverse reactions occurred in 38% of patients treated with FRUZAQLA. Serious adverse reactions in ≥2% of patients treated with FRUZAQLA included hemorrhage (2.2%) and gastrointestinal perforation (2.0%). Fatal adverse reaction(s) occurred in 14 (3.1%) patients who received FRUZAQLA. Fatal adverse reactions occurring in ≥2 patients include pneumonia (n=3), sepsis/septic shock (n=2), and hepatic failure/encephalopathy (n=2).
Adverse reactions leading to treatment discontinuation occurred in 20% of patients treated with FRUZAQLA. Adverse reactions leading to treatment discontinuations of FRUZAQLA in ≥1% of patients were asthenia and gastrointestinal perforation.
Dose interruptions of FRUZAQLA due to an adverse reaction occurred in 47% of patients. Adverse reactions leading to dose interruptions of FRUZAQLA in ≥2% of patients were PPE, proteinuria, asthenia, abdominal pain, hypertension, vomiting, and diarrhea.
Dose reductions of FRUZAQLA due to an adverse reaction occurred in 24% of patients. Adverse reactions leading to dose reductions of FRUZAQLA in ≥2% of patients were PPE, hypertension and asthenia.
Table 3 summarizes the adverse reactions in FRESCO-2.
Table 3: Adverse Reactions (≥10%) in Patients who Received FRUZAQLA and with a Difference Between Arms of ≥5% Compared to Placebo in FRESCO-2 (All Grades)
| Adverse Reaction | FRUZAQLA (N=456) | Placebo (N=230) | ||
| All Grades (%) | Grade 3 or 4 (%) | All Grades (%) | Grade 3 or 4 (%) | |
| General | ||||
| Fatigue1 | 53 | 12 | 39 | 4.8 |
| Vascular | ||||
| Hypertension1 | 38 | 14 | 9 | 0.9 |
| Gastrointestinal | ||||
| Stomatitis1 | 31 | 2.2 | 7.8 | 0.4 |
| Abdominal Pain1 | 25 | 3.5 | 20 | 3 |
| Diarrhea1 | 24 | 3.7 | 11 | 0 |
| Endocrine Disorders | ||||
| Hypothyroidism | 21 | 0.4 | 0.4 | 0 |
| Skin and Subcutaneous | ||||
| Palmar-plantar erythrodysesthesia (hand-foot skin reactions) | 19 | 6 | 2.6 | 0 |
| Renal | ||||
| Proteinuria1 | 18 | 1.8 | 5 | 0.9 |
| Respiratory | ||||
| Dysphonia1 | 18 | 0 | 5 | 0 |
| Musculoskeletal | ||||
| Musculoskeletal Pain1 | 16 | 1.1 | 7 | 0 |
| Arthralgia | 11 | 0.9 | 4.3 | 0 |
1 Represents a composite of multiple related terms.
Other important adverse reactions (all grades) that occurred in <10% of patients treated with FRUZAQLA included urinary tract infection (4.6%), epistaxis (3.9%), proctalgia (3.5%), pneumonia (2.4%), gastrointestinal hemorrhage (1.5%), gastrointestinal perforation (1.3%), thrombotic microangiopathy (0.2%), and posterior reversible encephalopathy syndrome (0.2%).
Table 4 provides laboratory abnormalities observed in FRESCO-2.
Table 4: Select Laboratory Abnormalities Worsening from Baseline Occurring in ≥20% of Patients in FRESCO-2
| Laboratory1 Abnormality | FRUZAQLA (N=456)2 | Placebo (N=230)2 | ||
| All Grade (%) | Grade 3 or 4 (%) | All Grades (%) | Grade 3 or 4 (%) | |
| Chemistry | ||||
| Triglycerides Increased | 53 | 2.8 | 22 | 1.0 |
| Cholesterol Increased | 37 | 1.9 | 22 | 1.9 |
| Aspartate Aminotransferase Increased | 36 | 4.3 | 24 | 1.9 |
| Albumin Decreased | 35 | 1.6 | 32 | 1.4 |
| Sodium Decreased | 35 | 1.1 | 27 | 0.9 |
| Alanine Aminotransferase Increased | 34 | 5 | 22 | 1.4 |
| Bilirubin Increased | 30 | 7 | 21 | 8 |
| Alkaline Phosphatase Increased | 20 | 1.6 | 27 | 0.5 |
| Magnesium Decreased | 20 | 0.5 | 10 | 0.5 |
| Hematology | ||||
| Lymphocytes Decreased | 30 | 6 | 32 | 4.7 |
| Platelets Decreased | 30 | 0.2 | 4.7 | 0 |
| Activated Partial Thromboplastin Time Increased | 21 | 2.7 | 18 | 1.5 |
1 Graded according to NCI CTCAE version 5.0.
2 Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory
measurement available: FRUZAQLA (range: 409-444) and placebo (range: 195-216).
FRESCO Study
The safety of FRUZAQLA was evaluated in FRESCO, a randomized, double-blind, placebo-controlled
study [see Clinical Studies (14.1)]. Patients received either FRUZAQLA 5 mg daily for the first
21 days of each 28-day cycle plus BSC (n=278) or matching placebo plus BSC (n=137).
The median duration of therapy with FRUZAQLA was 3.68 months (range: 0.3 to 22.1 months).
Serious adverse reactions occurred in 15% of patients treated with FRUZAQLA. Serious adverse reactions in ≥2% of patients included intestinal obstruction (2.9%) and hemorrhage (2.2%). Fatal adverse reaction(s) occurred in 7 (2.5%) patients who received FRUZAQLA including cerebral infarction (n=1), gastrointestinal hemorrhage (n=1), hemoptysis (n=1), bacterial infection (n=1), lung/lower respiratory infection (n=2), and multiple organ dysfunction (n=1).
Adverse reactions leading to treatment discontinuation occurred in 15% of patients who received FRUZAQLA. Adverse reactions leading to treatment discontinuations of FRUZAQLA in ≥1% were intestinal obstruction, proteinuria and hepatic function abnormalities.
Dose interruptions of FRUZAQLA due to an adverse reaction occurred in 35% of patients. Adverse reactions leading to dose interruptions of FRUZAQLA in ≥2% of patients were PPE, proteinuria, platelet count decreased, ALT increased, hypertension, and diarrhea.
Dose reductions of FRUZAQLA due to an adverse reaction occurred in 24% of patients. Adverse reactions leading to dose reduction of FRUZAQLA in ≥2% of patients were PPE, proteinuria, and hypertension.
Table 5 summarizes the adverse reactions in FRESCO.
Table 5: Adverse Reactions (≥10%) in Patients who Received FRUZAQLA and with a Difference Between Arms of ≥5% Compared to Placebo in FRESCO (All Grades)
| Adverse Reaction | Fruquintinib (N=278) | Placebo (N=137) | ||
| All Grades (%) | Grade 3 or 4 (%) | All Grades (%) | Grade 3 or 4 (%) | |
| Vascular | ||||
| Hypertension1 | 61 | 23 | 17 | 2.2 |
| Hemorrhage1 | 28 | 1.1 | 14 | 0 |
| Renal | ||||
| Proteinuria1 | 55 | 4.7 | 30 | 0 |
| Skin and Subcutaneous | ||||
| Palmar-plantar erythrodysesthesia (hand-foot skin reactions) | 49 | 11 | 2.9 | 0 |
| Respiratory | ||||
| Dysphonia1 | 38 | 0 | 1.5 | 0 |
| Throat Pain | 10 | 0 | 1.5 | 0 |
| Gastrointestinal | ||||
| Stomatitis1 | 33 | 0.7 | 2.9 | 0 |
| Abdominal Pain1 | 29 | 4 | 17 | 1.5 |
| Diarrhea1 | 25 | 3.6 | 5 | 0 |
| General | ||||
| Fatigue1 | 25 | 2.5 | 13 | 1.5 |
| Metabolism | ||||
| Anorexia1 | 21 | 1.4 | 9 | 0 |
| Musculoskeletal | ||||
| Musculoskeletal Pain1 | 22 | 2.2 | 6 | 1.5 |
| Back Pain | 15 | 1.8 | 7 | 0 |
| Arthralgia | 13 | 0.4 | 2.2 | 0 |
| Endocrine Disorders | ||||
| Hypothyroidism | 17 | 0 | 2.2 | 0 |
1 Represents a composite of multiple related terms.
Other clinically important adverse reactions (all grades) that occurred in <10% of patients treated with FRUZAQLA included urinary tract infection (9%), rash (9%), upper respiratory tract infection (4.7%), proctalgia (3.6%), pneumonia (2.9%), and gastrointestinal perforation or fistula (2.2%).
Table 6 provides laboratory abnormalities observed in FRESCO.
Table 6: Select Laboratory Abnormalities Worsening from Baseline Occurring in ≥20% of Patients in FRESCO
| Laboratory1 Abnormality | FRUZAQLA (N=278)2 | Placebo (N=137)2 | ||
| All Grades (%) | Grade 3 or 4 (%) | All Grades (%) | Grade 3 or 4 (%) | |
| Chemistry | ||||
| Creatinine Increased | 87 | 0.7 | 75 | 1.5 |
| Glucose Increased | 43 | 1.1 | 31 | 3.0 |
| Aspartate Aminotransferase Increased | 42 | 3.6 | 31 | 1.5 |
| Alkaline Phosphatase Increased | 40 | 4.3 | 34 | 6 |
| Bilirubin Increased | 39 | 4.7 | 34 | 8 |
| Alanine Aminotransferase Increased | 33 | 2.2 | 18 | 1.5 |
| Sodium Decreased | 33 | 6 | 31 | 5 |
| Urate Increased | 26 | 26 | 22 | 22 |
| Calcium Decreased | 25 | 0.4 | 13 | 0 |
| Potassium Decreased | 22 | 1.8 | 15 | 2.3 |
| Hematology | ||||
| Platelets Decreased | 29 | 3.6 | 6 | 0.7 |
| Hemoglobin Decreased | 23 | 0.7 | 33 | 4.5 |
1 Graded according to NCI CTCAE version 4.03.
2 Each test incidence is based on the number of patients who had both baseline and at least one on-study laboratory measurement available: FRUZAQLA (range: 257-277) and placebo (range: 126-134).
7 DRUG INTERACTIONS
7.1 Effects of Other Drugs on FRUZAQLA
Strong CYP3A Inducers
Avoid concomitant use of drugs that are strong CYP3A inducers with FRUZAQLA.
Concomitant use with a strong CYP3A inducer may decrease fruquintinib Cmax and AUC [see Clinical Pharmacology (12.3)], which may reduce the efficacy of FRUZAQLA.
Moderate CYP3A Inducers
If possible, avoid concomitant use of drugs that are moderate CYP3A inducers with FRUZAQLA. If it is not possible to avoid concomitant use of a moderate CYP3A inducer and fruquintinib, continue to administer FRUZAQLA at the recommended dosage.
Concomitant use with a moderate CYP3A inducer may decrease fruquintinib Cmax and AUC [see Clinical Pharmacology (12.3)], which may reduce the efficacy of FRUZAQLA.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on findings in animal studies and its mechanism of action, FRUZAQLA can cause fetal harm when administered to a pregnant woman. In an embryo-fetal developmental study in pregnant rats, oral administration of fruquintinib during the period of organogenesis resulted in teratogenicity and embryo lethality at exposures below the clinical exposure (see Data). There are no data on the use of FRUZAQLA in pregnant women. Advise pregnant women of the potential risk to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
In an embryo-fetal developmental study in pregnant rats, daily oral administration of fruquintinib at doses ≥0.1 mg/kg [approximately 0.2 times the recommended clinical dose of 5 mg based on body surface area (BSA)] during the period of organogenesis resulted in fetal external (edema and head and tail abnormalities), visceral, and skeletal malformations. At doses of 0.25 mg/kg (approximately 0.5 times the recommended clinical dose of 5 mg based on BSA), an increase in postimplantation loss and reduction in live fetuses was observed.
8.2 Lactation
Risk Summary
There are no data regarding the presence of fruquintinib or its metabolites in human milk or its effects on a breastfed child or on milk production. Because of the potential for serious adverse reactions in the breastfed child, advise women not to breastfeed during treatment with FRUZAQLA and for 2 weeks after the last dose.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify pregnancy status of females of reproductive potential prior to initiating FRUZAQLA.
Contraception
Females and Males
Females of childbearing potential and males with female partners of childbearing potential should use effective contraception during treatment and for 2 weeks after the last dose of FRUZAQLA [see Warnings and Precautions (5.11) and Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and efficacy of FRUZAQLA in patients younger than 18 years of age have not been established.
8.5 Geriatric Use
In FRESCO-2, 212 (46%) patients who received FRUZAQLA were ≥65 years of age and older, of whom 43 (20%) of patients were ≥75 years. There were no observed overall differences in safety and effectiveness of FRUZAQLA in geriatric compared to younger patients.
Of the total number of FRUZAQLA-treated patients in the FRESCO study, 50 (18%) were 65 years of age and older, and one patient was ≥75 years. There were no observed overall differences in safety and effectiveness of FRUZAQLA in geriatric compared to younger patients.
8.6 Hepatic Impairment
No dosage adjustment is recommended for patients with mild hepatic impairment (total bilirubin less than or equal to the ULN with AST greater than ULN or total bilirubin greater than 1 to 1.5 times ULN with any AST [see Clinical Pharmacology (12.3)].
FRUZAQLA has not been sufficiently studied in patients with moderate hepatic impairment (total bilirubin greater than 1.5 times and less than 3 times ULN and any AST). FRUZAQLA is not recommended for use in patients with severe hepatic impairment (total bilirubin greater than 3 times ULN and any AST).
11 DESCRIPTION
Fruquintinib is a kinase inhibitor with the chemical name 6-[(6,7-dimethoxyquinazolin-4-yl)oxy]-N,2- dimethyl-1-benzofuran-3-carboxamide. Its molecular formula is C21H19N3O5, which corresponds to a molecular weight of 393.39 g/mol. Fruquintinib has the following chemical structure:
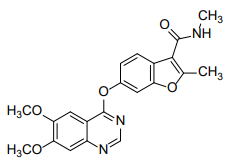
Fruquintinib is a white to off-white powder with a dissociation constant (pKa) of 2.78. The aqueous solubility of fruquintinib is pH-dependent with a solubility of 0.9 μg/mL at pH 6.8 that increases under acidic conditions to 129.9 μg/mL at pH 1.
FRUZAQLA (fruquintinib) capsules for oral administration contain 1 mg or 5 mg of fruquintinib. The inactive ingredients are corn starch, microcrystalline cellulose, and talc. The 1 mg capsule shell contains FD&C Yellow No. 5 (tartrazine), FD&C Yellow No. 6 (sunset yellow FCF), gelatin, and titanium dioxide. The 5 mg capsule shell contains FD&C Blue No. 1 (brilliant blue FCF), FD&C Red No. 40 (allura red AC), gelatin, and titanium dioxide. The printing ink for 1 mg and 5 mg capsules contains butanol, dehydrated alcohol, ferrosoferric oxide, isopropyl alcohol, potassium hydroxide, propylene glycol, purified water, shellac and strong ammonia solution.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Fruquintinib is a small molecule kinase inhibitor of vascular endothelial growth factor receptors (VEGFR)-1, -2, and -3 with IC50 values of 33, 35, and 0.5 nM, respectively. In vitro studies showed fruquintinib inhibited VEGF-mediated endothelial cell proliferation and tubular formation. In vitro and in vivo studies showed fruquintinib inhibited VEGF-induced VEGFR-2 phosphorylation. In vivo studies showed fruquintinib inhibited tumor growth in a tumor xenograft mouse model of colon cancer.
12.2 Pharmacodynamics
Fruquintinib exposure-response relationships and the time course of pharmacodynamic response are unknown.
Cardiac Electrophysiology
A mean increase in QTc interval >20 milliseconds (ms) was not observed at the approved recommended dosage.
12.3 Pharmacokinetics
The fruquintinib steady-state geometric mean (% coefficient of variation [CV]) maximum concentration (Cmax) is 300 ng/mL (28%) and area under the concentration-time curve for the dosing interval (AUC0-24h) is 5880 ng∙h/mL (29%) at the recommended dosage. The fruquintinib Cmax and AUC0-24h are dose-proportional across the dosage range of 1 to 6 mg (0.2 to 1.2 times the recommended dosage). Fruquintinib steady state is achieved after 14 days with a mean AUC0-24h accumulation of 4-fold.
Absorption
The fruquintinib median (min, max) time to Cmax is approximately 2 hours (0, 26 hours).
Effect of Food
No clinically significant differences in fruquintinib pharmacokinetics were observed following administration of a high-fat meal (800 to 1000 calories, 50% fat).
Distribution
The mean (SD) apparent volume of distribution of fruquintinib is approximately 46 (13) L. Plasma protein binding of fruquintinib is approximately 95%.
Elimination
The fruquintinib mean (SD) elimination half-life is approximately 42 (11) hours and the apparent clearance is 14.8 (4.4) mL/min.
Metabolism
Fruquintinib is primarily eliminated by CYP450 and non-CYP450 (i.e., sulfation and glucuronidation) metabolism. CYP3A and to a lesser extent CYP2C8, CYP2C9, and CYP2C19 are the CYP450 enzymes involved in fruquintinib metabolism.
Excretion
Following oral administration of a 5 mg radiolabeled fruquintinib dose, approximately 60% of the dose was recovered in urine (0.5% unchanged) and 30% of the dose was recovered in feces (5% unchanged).
Specific Populations
No clinically significant differences in the pharmacokinetics of fruquintinib were observed based on age (18 to 82 years), sex, race (Asian, Black, and White), ethnicity (Hispanic/Latino vs.
non-Hispanic/Latino), body weight (48 to 108 kg), mild to moderate renal impairment (CrCL 30 to
89 mL/min), mild hepatic impairment (total bilirubin less than or equal to ULN with AST greater than ULN or total bilirubin greater than 1 to 1.5 times ULN with any AST).
The effect of moderate to severe hepatic impairment (total bilirubin greater than 1.5 times ULN and any AST) on fruquintinib pharmacokinetics is unknown.
Drug Interaction Studies
Clinical Studies and Model-Informed Approaches
Strong CYP3A inducers: Fruquintinib Cmax decreased by 12% and AUCinf by 65% following concomitant use with rifampin (strong CYP3A inducer).
Moderate CYP3A inducers: Fruquintinib Cmax is predicted to decrease by 4% and AUCinf by 32% following concomitant use with efavirenz (moderate CYP3A inducer).
Other Drugs: No clinically significant differences in fruquintinib pharmacokinetics were observed when used concomitantly with itraconazole (strong CYP3A inhibitor) or rabeprazole (proton pump inhibitor; gastric acid reducing agent).
No clinically significant differences in the pharmacokinetics of the following drugs were observed when used concomitantly with fruquintinib: dabigatran etexilate (P-gp substrate), or rosuvastatin (BCRP substrate).
In Vitro Studies
Cytochrome P450 Enzymes: Fruquintinib is not an inhibitor of CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6 and CYP3A, or an inducer of CYP1A2, CYP2B6, CYP3A.
Transporter Systems: Fruquintinib is not a substrate of P-glycoprotein (P-gp), organic anion transporting polypeptide (OATP)1B1 or OATP1B3. Fruquintinib is not an inhibitor of OATP1B1, OATP1B3, organic anion transporter (OAT)1, OAT3, organic cation transporter (OCT)2, multidrug and toxin extrusion protein (MATE)1, or MATE2-K.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies have not been conducted with fruquintinib.
Fruquintinib was not mutagenic in the in vitro bacterial reverse mutation (Ames) assay or clastogenic in the in vitro Chinese hamster ovary chromosome aberration assay. Fruquintinib was not genotoxic in the in vivo rat micronucleus or alkaline comet assays.
13.2 Animal Toxicology and/or Pharmacology
In repeat dose toxicity studies in rats, daily oral administration of fruquintinib at doses ≥0.6 mg/kg (approximately 1.2 times the recommended clinical dose of 5 mg based on BSA) resulted in broken or lost teeth.
14 CLINICAL STUDIES
14.1 Metastatic Colorectal Cancer
FRESCO-2 Study
The efficacy of FRUZAQLA was evaluated in FRESCO-2 (NCT04322539), an international, multicenter, randomized, double-blind, placebo-controlled study that enrolled 691 patients with metastatic colorectal cancer who had disease progression during or after prior treatment with fluoropyrimidine-, oxaliplatin-, irinotecan-based chemotherapy, an anti-VEGF biological therapy, if RAS wild type, an anti-EGFR biological therapy, and trifluridine/tipiracil, regorafenib, or both. Patients with an ECOG PS ≥2, left ventricular fraction ≤50%, systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg, urine protein ≥1 g/24h, or untreated brain metastases were ineligible. Randomization was stratified by prior use of trifluridine/tipiracil or regorafenib (trifluridine/tipiracil vs. regorafenib vs. trifluridine/tipiracil and regorafenib), RAS status (wild type vs. mutant), and duration of metastatic disease (≤18 months vs. 18 months).
Patients were randomized (2:1) to receive FRUZAQLA 5 mg orally once daily (N=461) for the first 21 days of each 28-day cycle plus BSC or placebo (N=230) plus BSC. Patients received either FRUZAQLA or placebo until disease progression or unacceptable toxicity. The major efficacy outcome measure was overall survival (OS) and an additional efficacy outcome measure was progression-free survival (PFS) as determined by investigators according to RECIST v1.1.
The study population characteristics were median age of 64 years (range: 25 to 86), with 47% ≥65 years of age; 56% male; 81% White, 9% Asian, 2.9% Black or African American, and 0.7% Native Hawaiian/Pacific Islander; 43% had an ECOG PS of 0 and 57% had an ECOG PS of 1, and 63% had RAS-mutant tumors. Eighteen percent of the patients were enrolled in North America, 72% in Europe, and 10% in Asia Pacific (Japan and Australia) region.
All patients received prior treatment with fluoropyrimidine, oxaliplatin, and irinotecan-based chemotherapy; 96% received prior anti-VEGF therapy, 39% received prior anti-EGFR therapy, 91% received trifluridine/tipiracil, 48% received regorafenib, and 39% received both trifluridine/tipiracil and regorafenib.
The addition of FRUZAQLA to BSC resulted in a statistically significant improvement in OS and PFS compared to placebo plus BSC (see Table 7, Figure 1).
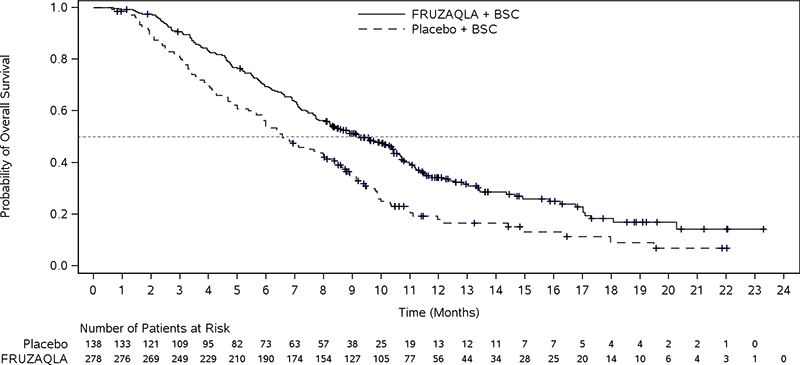
FRESCO Study
The efficacy of FRUZAQLA was evaluated in FRESCO (NCT02314819), a multicenter, randomized, double-blind, placebo-controlled study conducted in China that enrolled 416 patients with metastatic colorectal cancer who had disease progression during or after prior treatment with fluoropyrimidine-, oxaliplatin, or irinotecan-based chemotherapy. Patients older than 75 years of age, Eastern Cooperative Oncology Group (ECOG) performance status (PS) ≥2, left ventricular ejection
fraction ≤50%, systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg, urine protein ≥1 g/24h, or brain metastases were ineligible. Randomization was stratified by prior use of VEGF inhibitors (yes vs. no) and K-RAS status (wild type vs. mutant).
Patients were randomized (2:1) to receive FRUZAQLA 5 mg orally once daily (N=278) for the first 21 days of each 28-day cycle plus BSC or placebo (N=138) plus BSC. Patients received either FRUZAQLA or placebo until disease progression or unacceptable toxicity. The major efficacy outcome measure was OS and an additional efficacy outcome measure was PFS as determined by investigators according to RECIST v1.1.
The study population characteristics were median age of 56 years (range: 23 to 75), with 19% ≥65 years of age; 61% male; 100% Asian; 27% had an ECOG PS of 0 and 73% had an ECOG PS of 1 (73%), and 44% had K-RAS mutant tumors.
All patients received prior treatment with fluoropyrimidine-, oxaliplatin- and irinotecan-based chemotherapy; 30% of patients received prior anti-VEGF therapy, and 14% received prior anti-EGFR therapy.
The addition of FRUZAQLA to BSC resulted in a statistically significant improvement in OS compared to placebo plus BSC (see Table 7, Figure 2).
Table 7: Efficacy Results from FRESCO-2 and FRESCO Studies
| FRESCO-2 | FRESCO | |||
| Endpoint | FRUZAQLA + BSC N=461 | Placebo + BSC N=230 | FRUZAQLA + BSC N=278 | Placebo + BSC N=138 |
| OS | ||||
| Number of patients with event (%) | 317 (69%) | 173 (75%) | 188 (68%) | 109 (79%) |
| Median in months (95% CI) | 7.4 (6.7, 8.2) | 4.8 (4.0, 5.8) | 9.3 (8.2, 10.5) | 6.6 (5.9, 8.1) |
|
Hazard Ratioa (95% CI) |
0.66 (0.55, 0.80) | 0.65 (0.51, 0.83) | ||
| P-Valueb | <0.001 | <0.001 | ||
| PFS | ||||
| Number of patients with event (%) | 392 (85%) | 213 (93%) | 235 (85%) | 125 (91%) |
| Median in months (95% CI) | 3.7 (3.5, 3.8) | 1.8 (1.8, 1.9) | 3.7 (3.7,4.6) | 1.8 (1.8, 1.8) |
|
Hazard Ratioa (95% CI) |
0.32 (0.27, 0.39) | 0.26 (0.21, 0.34) | ||
| P-Valuebc | <0.001 | - | ||
Abbreviations: CI=confidence interval; N=number of patients; OS=overall survival; PFS=progression-free survival
a The Hazard Ratio and its 95% CI were estimated using a stratified Cox proportional hazards model.
b P-Value (2-sided) was calculated using a stratified log-rank test.
c P-Value for the PFS analysis in FRESCO was not included due to lack of multiplicity adjustment for this analysis.
Figure 1: Kaplan-Meier Curve for Overall Survival in FRESCO-2
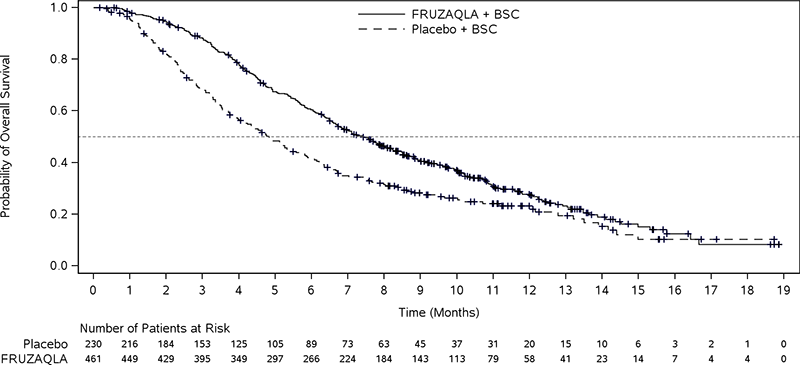
Figure 2: Kaplan-Meier Curve for Overall Survival in FRESCO
16HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
| Capsule Strength | Description | Package Configuration | NDC Number |
| 1 mg | Size 3 hard gelatin capsule with yellow opaque cap and white opaque body, imprinted with “HM013” over “1 mg” on the body in black ink | White high-density polyethylene (HDPE) bottle with child-resistant closure packaged in a carton. Each bottle contains 21 capsules. | 63020-210-21 |
| 5 mg | Size 1 hard gelatin capsule with a red opaque cap and white opaque body, imprinted with “HM013” over “5 mg” on the body in black ink | 63020-225-21 |
Storage and handling
Store at 20°C to 25°C (68°F to 77°F). Brief exposure to 15°C and 30°C (59°F to 86°F) permitted (see USP Controlled Room Temperature).
Any unused medicinal product or waste material should be disposed of in accordance with local requirements.
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Hypertension
Advise patients to undergo regular blood pressure monitoring and to contact their health care provider if blood pressure is elevated or if symptoms from hypertension occur including severe headache, lightheadedness, or new neurologic symptoms [see Warnings and Precautions (5.1)].
Hemorrhages
Advise patients that FRUZAQLA may increase the risk of bleeding and to contact their healthcare provider for unusual, severe, or persistent bleeding, bruising, or symptoms of bleeding, such as lightheadedness [see Warnings and Precautions (5.2)].
Infections
Advise patients to contact their healthcare provider if they experience signs and symptoms of infection [see Warnings and Precautions (5.3)].
Gastrointestinal Perforation
Advise patients to contact a healthcare provider immediately if they experience severe abdominal pains, or other symptoms of gastrointestinal perforation or fistula [see Warnings and Precautions (5.4)].
Hepatotoxicity
Advise patients that they will need to undergo laboratory tests to monitor liver function and to report any new symptoms indicating hepatic toxicity or failure [see Warnings and Precautions (5.5)].
Proteinuria
Advise patients that they will need to undergo laboratory tests to monitor for proteinuria and to contact their healthcare provider for signs or symptoms of proteinuria [see Warnings and Precautions (5.6)].
Palmar-plantar erythrodysesthesia (PPE)
Advise patients to contact their healthcare provider for progressive or intolerable rash [see Warnings and Precautions (5.7)].
Posterior Reversible Encephalopathy Syndrome (PRES)
Advise patients to immediately contact their healthcare provider for new onset or worsening neurological function [see Warnings and Precautions (5.8)].
Impaired Wound Healing
Advise patients that FRUZAQLA may impair wound healing. Advise patients to inform their healthcare provider of any planned surgical procedure [see Warnings and Precautions (5.9)].
Arterial Thrombosis
Advise patients to seek immediate medical attention for new onset chest pain or acute neurologic symptoms consistent with myocardial infarction or stroke [see Warnings and Precautions (5.10)].
Allergic Reactions to FD&C Yellow No. 5 (Tartrazine) and No. 6 (Sunset Yellow FCF)
Advise patients that FRUZAQLA 1 mg contains FD&C Yellow No. 5 (tartrazine), which may cause allergic-type reactions (including bronchial asthma) in certain susceptible persons or in patients who also have aspirin hypersensitivity [see Warnings and Precautions (5.11)].
Advise patients FRUZAQLA 1 mg contains FD&C Yellow No. 6 (sunset yellow FCF) which may cause allergic-type reactions [see Warnings and Precautions (5.11)].
Embryo-Fetal Toxicity
Advise females to inform their healthcare provider if they are pregnant or become pregnant. Inform females of the risk to a fetus and potential loss of pregnancy [see Warnings and Precautions (5.12) and Use in Specific Populations (8.1)].
Advise females of reproductive potential to use effective contraception during treatment and for 2 weeks after the last dose of FRUZAQLA [see Warnings and Precautions (5.12) and Use in Specific Populations (8.3)].
Advise males with female partners of reproductive potential to use effective contraception during treatment and for 2 weeks following the last dose of FRUZAQLA [see Warnings and Precautions (5.11) and Use in Specific Populations (8.3)].
Lactation
Advise patients not to breastfeed during treatment with FRUZAQLA and for 2 weeks after the last dose of FRUZAQLA [see Use in Specific Populations (8.2)].
